Post-Market Evaluation for the Safety of Laparoscopic Power Morcellator
Post-Market Evaluation for the Safety of Laparoscopic Power Morcellator
Laparoscopic power morcellator (LPM) are surgical instruments used in minimally invasive abdominal procedures such as, laparoscopic hysterectomies and fibroid removal [4]. LPMs were first introduced in 1991, which were designed in the shape of a drill with sharp blades at the end, and classified as class II medical devices. The device provides quicker recovery, less post-operative pain and fewer wound complications [5]Laparoscopic power morcellators work through minimally invasive incisions to remove the uterine fibroids by shredding them into small pieces, which leaves behind tissue debris for the vacuum system to extract out of the body [4]. Recently, and due to a believe that cancer cells may still remain in the body following certain uterine surgical procedures in patients with fibroids, a containment system was introduced to isolate the morcellated tissue from the body, and thus, prevent the spread of morcellated tissue through the abdominal cavity [4]This study was designed to fulfill two main objectives, which are:
- Evaluate the current practice of using LPM in Saudi healthcare facilities, and
- Test the awareness of the device users of the LPM risk of spreading cancer cells following uterine surgical procedures, and whether or not the manufacturer recommendation of using a containment system is followed.
LPMs are devices that are used during minimally invasive surgeries to shred tissue into small pieces that can be removed through a very small incision site. The device can be used for the removal of the abdominal organs, i.e. gallbladder, kidney, liver, and spleen. Furthermore, it is commonly used in the uterus removal surgical procedures, which include hysterectomy, the surgical procedure of the uterus removal, and myomectomy, the surgical procedure of the uterine fibroids removal [4].
Uterine fibroids refer to non-cancerous growths in uterus, while uterine sarcomas, on the other hand, are cancerous cells, and these two conditions are difficult to distinguished with available tests. According to the US FDA, uterine sarcomas are more frequent than previously estimated. Thus, when using an LPM for myomectomy or hysterectomy in women with assumed uterine fibroids that are essentially uterine sarcomas, the procedure would pose a risk of spreading cancer cells beyond the uterus. These findings are assumed to lower the patient chance of long-term survival without cancer [4], which add to the myomectomy or hysterectomy post-operation complications, and require certain actions, i.e. utilizing a containment system, to protect the patient safety.
In reference to a review published by the US FDA by 2014, 1 in 350 women who undergo morcellation for hysterectomy or myomectomy could essentially have uterine sarcomas, the rate that is much higher than previously estimated rate of 1 in 10,000 [1].
In 2017, another white paper was published to tackle the issue of spreading cancer cells by LPMs, which included more studies and estimated rates of 1 in 225 to 1 in 580 women who undergo fibroid removal may have uterine sarcomas [4]. The process of morcellation could shred some cancerous cells causing them to disperse faster, resulting in an upstage of the hidden uterine cancer from stage one up to stage four, and thus, reduce the chances of survival and the possibility of treatment [4].
On the other hand, and with respect to the medical device reports, the same study indicated that, and as of April 2017, a total of 262 reports were submitted to the FDA database. These reports described the spreading of cancer cells in association with LPMs, with 18 reports that claimed upstaging the cancer after the morcellator surgery [4].
In order to meet the objectives of this study the following steps were accomplished:
- A screening over the SFDA database was conducted to figure out the manufacturers that are authorized to distribute laparoscopic power morcellators in the Saudi market [6].
- The authorized representative of each manufacturer was then contacted to report the Saudi sites that have the device in question.
The SFDA officer of each Saudi healthcare facility was then requested to fulfill a survey that was designed to meet the study objectives. The developed survey contained 8 specific questions regarding the device in question, which are illustrated in figure 1.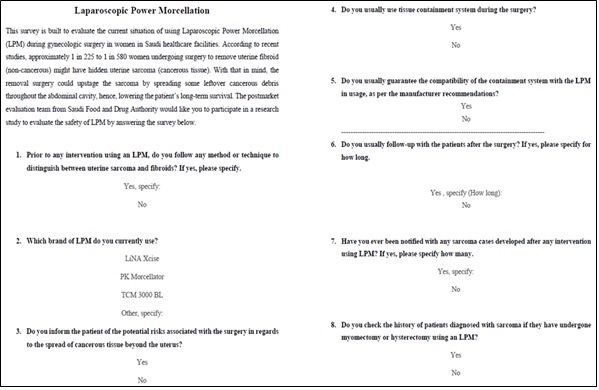
Figure 1. The study survey that was developed to evaluate the safety of LPM.
Part II: Results
- The market analysis revealed a total of 16 Saudi healthcare facilities that have LPM in use.
- 50% of the surveyed Saudi healthcare facilities are not following any method or technique to ensure and validate the absence of malignancy prior to the surgical procedures of hysterectomy or myomectomy procedure using an LPM.
- 50% of the surveyed Saudi healthcare facilities, are unaware of the importance of using containment system to reduce the risk of spreading cancer tissue in the abdominal cavity.
25% of the population do not even follow up with patients after the surgery, which may jeopardize the welfare of patients by being unaware of the patients’ status.
- So far Saudi healthcare facilities reported zero cases of developed sarcoma following a hysterectomy or myomectomy surgeries using power morcellators. However, 25% of the surveyed healthcare facilities usually do not check the history of patients diagnosed with sarcoma to establish a relationship between the two cases.
Part III: Conclusion
Due to the laparoscopic power morcellation potential risk of spreading unsuspected cancerous tissue, notably uterine sarcomas, beyond the uterus, following hysterectomy or myomectomy surgery procedures, SFDA would like to bring the attention of healthcare providers to the following recommendations.
Recommendations for healthcare providers:
- Make sure to use laparoscopic power morcellation with an authorized laparoscopic power morcellation containment system, whenever you decide that morcellation is appropriate.
- Make sure that the laparoscopic power morcellation containment system is compatible with the utilized laparoscopic power morcellator.
Make sure to discuss the risks and benefits of all relevant treatment options with your patients, informing them about the potential risk associated with the morcellation
- surgeries, and that the use of laparoscopic power morcellators during fibroid surgery may spread cancer and decrease their long-term survival.
- Make sure to conduct a thorough preoperative screening, and not to use laparoscopic power morcellators in cases when the intended morcellated tissue is known or suspected to be malignant.
- In reference to current recommendations revealed by international regulatory agencies, it is recommended that the use of laparoscopic power morcellation is limited to certain appropriately selected women undergoing myomectomy or hysterectomy. Recent reports also highlighted that the risk of spreading cancer cells is increased when using laparoscopic power morcellators for removal of uterine tissue containing suspected fibroids in patients who are post-menopausal, or over 50 years of age, or candidates for removal of tissue (en bloc) through the vagina or via a mini-laparotomy incision. Furthermore, uncontained power morcellation is expected to be associated with the spread of benign uterine tissue, i.e. parasitic myomas and disseminated peritoneal leiomyomatosis, which would possibly require additional surgeries.
Make sure to report any adverse event you notice with laparoscopic power morcellators through the National Center for Medical Devices Reporting (NCMDR) system: https://ncmdr.sfda.gov.sa, the Saudi Vigilance System https://ade.sfda.gov.sa, or the SFDA call center: 19999
Recommendations for SFDA Actions:
- Issuing a safety communication with the above mentioned recommendations to raise the awareness of device users in the Saudi market.
- Following-up with the manufacturers to ensure that each LPM manufacturer is in-compliance with the previous SFDA recommendations in regards to include a warning box on the device label to highlight the need to utilize a containment system, which was previously directed to LPM manufacturers.
Prior to the authorization of new laparoscopic power morcellators in the Saudi market, it is recommended to check that the device labeling highlights specific gynecologic indications. Such indication are to include a boxed warning, contraindications, and warnings regarding
- the risk of use related to age, spreading malignant and benign uterine tissue, and the use of laparoscopic power morcellators containment systems, as provided in the guidance: "Product Labeling for Laparoscopic Power Morcellators" [3].
Laparoscopic power morcellator manufacturers SHALL develop a plan to raise the awareness of the device users and healthcare practitioners to follow the recommended practices in gynecologic surgeries, as specified in the device Indications for Use.
Grateful thanks to Eng. Danah Alotaibi for designing, reviewing the up to date articles, and writing up the context of this study. Eng. Bader Aloufi verified the study methodology and supervised the study progress. With the appreciation to Rashed Abu Haimed, for drafting this summary and the post-market clinical evaluation team for their efforts in conducting this work.
For further information or inquiries related to this study, you may contact us at: cia.md@sfda.gov.sa
[1] FDA, "UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication," Food and Drug Authority, 24 11 2014. [Online].
[2] FDA, "UPDATE: Perform Only Contained Morcellation When Laparoscopic Power Morcellation Is Appropriate: FDA Safety Communication," The U.S. Food and Drug Administration (FDA), 29 12 2020. [Online].
[3] FDA, "Product Labeling for Laparoscopic Power Morcellators," U.S. Department of Health and Human Services; Food and Drug Administration; Center for Devices and Radiological Health, 2020.
[4] FDA, "Laparoscopic Power Morcellators," Food and Drug Authority, 25 02 2020. [Online].
[5] Michelle Llamas, "Power Morcellators," Drug Watch, 28 07 2020. [Online].
[6] Atheer Alamri, "Laparoscopic Power Morcellation (LPMs)," Saudi Food and Drug Authority, Riyadh, 2020.
[7] FDA, "UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication," FDA, 2014.


