Post-Market Evaluation for the Safety of Ventilator Associated Pneumonia in the Intensive Care Unit
Post-Market Evaluation for the Safety of Ventilator Associated Pneumonia in the Intensive Care Unit
The prevalence of ventilator-associated pneumonia (VAP) varies depending on several factors. The estimated prevalence is from 5-40%. This variation depends upon the infection seen in a particular country. In North America, the prevalence was low, with 1 to 2.5 cases per 1000 ventilator days. However, in the European countries, a higher rate of infection that was close to 18.3 cases in 1000 ventilator days, was reported. Still, much higher rates are seen in the lower-middle-income countries. However, in the last 2 decades, using a stable definition for VAP, the incidence of VAP is lesser and estimated to be nearly 10% in a population diagnosed with cardiac, respiratory infection, and surgical procedures. Accordingly, The Centers for Disease Control and Prevention’s National Healthcare Safety Network (NHSN) has reported large decreases in the incidence of VAP for both medical and surgical ICUs over the past 15 years [2].
Few studies reported the prevalence of VAP in KSA. A study by Balkhy et al. narrating the prevalence of various hospital-acquired infections listed VAP as the second most common infection (28.9%), which is much higher than reported globally [2]. Another study in pediatric patients reported 8.87 per 1,000 ventilation days with a ventilator utilization rate of 47%. In all these cases, the most associated microorganism was Pseudomonas aeruginosa (P.a) [3]. Another point prevalence reported a VAP prevalence of 27% [4]. Further, the prevalence of VAP associated with COVID-19 is yet to be reported in detail, although case reports and case studies are reported in a few publications.
However, this large variation between different countries is due to the definition of the disease followed, diagnostic criteria followed (novel diagnostic methods followed in the last decades), population group studied (type of disease patient suffering: cancer patients, trauma, aspiration resulting from brain injury and lung contusion, the increased incidence is seen with chronic obstructive pulmonary disease). A more common incidence seen with lung infection is due to the prolonged duration of mechanical ventilation, which leads to muscular weakness and increased incidence of micro-aspiration. This is seen exactly in acute respiratory distress syndrome (ARDS) with a higher incidence of up to 29% [2, 3, and 4].
The mortality rate for ventilator-associated pneumonia ranges from 20% to 50%. The morbidity here is related to the prolonged stay in ICU due to VAP. One study has reported that the patients with pneumonia stayed three times longer in the ICU (12 d versus 4.3 d, p < 0.001) and had 4-fold greater mortality than controls (20.3% versus 5.6%, p < 0.001) [5]. Another study reported an increased risk of death associated with the VAP (odds ratio [OR]: 2.0; 95%CI: 1.61 to 2.49) and the mean length of stay of cases was 34 d compared with 21 d for controls. The prolonged duration of mechanical ventilation and stay in the ICU were co-related and associated with the microorganism [6]. The reported mortality rate in KSA is 15.4% corresponding to 15.9 episodes per 1000 ventilator days. The rate decreased from 19.1 in 2003 to 6.3 per 1000 ventilator days in 2009. With the study reports, it is seen that the mortality rate is lower in KSA compared to globally [7].
The study was conducted to attain several main objectives:
1. To evaluate whether pneumonia infection is associated with using of Ventilator System, as indicated by several scientific literature.
2. To assess the level of safety and quality of the Ventilator System's current practices within Saudi healthcare providers' ICU.
The sampling technique implemented to obtain the sample size is a convenience sample. Where there was a predefined list of 450 HCFs in Saudi Arabia; however, only 55 healthcare facilities (HCF) were requested to fulfill the required questionnaire Based on their frequent use of the device. Figure 1 clarifies the geographical distribution of these sites within Saudi Arabia. In addition, The Saudi Epidemiological Society was also contacted, and they cooperated with us in distributing the questionnaire to the concerned users.
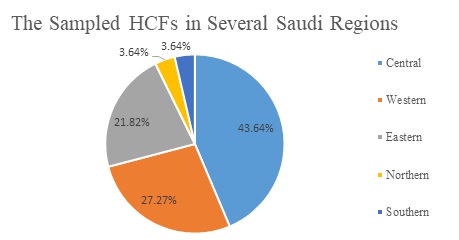
Figure 1: Demonstration of the geographical distribution of the sampled HCFs between Saudi regions
The questionnaire is segregated into two main sections: the first part covers 6 demographic queries about the healthcare profession, while the second part contains 9 specific inquiries about ventilator associated pneumonia infection. These questions structured by various formats, including open-ended and close-ended questions. In addition, all close-ended questions have mutually exclusive answers to avoid ambiguity. Not only that but also some questions have the option for multiple answers to be selected, which will provide more precise answers and shows some pattern idea.
Different microflora is associated with VAP. Various flora reported to be associated with the VAP is a mix of gram-positive cocci and gram-negative bacilli. Gram-positive cocci listed are oxacillin-susceptible Staphylococcus aureus (OSSA) and oxacillin-resistant Staphylococcus aureus (ORSA). Similarly, gram-negative bacilli listed among the VAP are Pseudomonas aeruginosa (P.a), Stenotrophomonas maltophilia, Klebsiella pneumonia, and Acinetobacter species. Among all these predominant gram-negative bacilli, Pseudomonas aeruginosa was considered a major microorganism, as shown by the respondents below in figure 2.
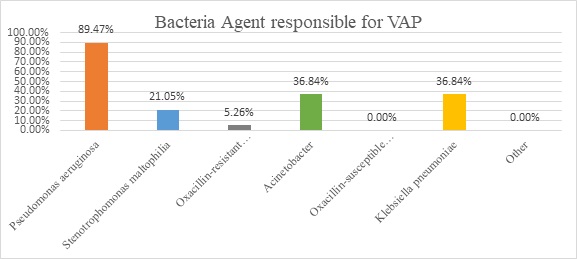
FIGURE 2: MOST ASSOCIATED PATHOGENS TO VAP.
4. Awareness Level of HCFs.
Multiple elements need to be measured to disclose the realization of the healthcare community regarding the importance of Reporting complaints related to medical devices, which helps in taking immediate corrective action, elevating the awareness of the potential risks of the device, and the way to prevent reoccurrences. Nevertheless, figure 3, as revealed by the respondents, demonstrates that 58% of healthcare practitioners did not report complaints cases of ventilator-associated pneumonia to the SFDA NCMDR that highlight the low level of awareness regarding regulatory practice.
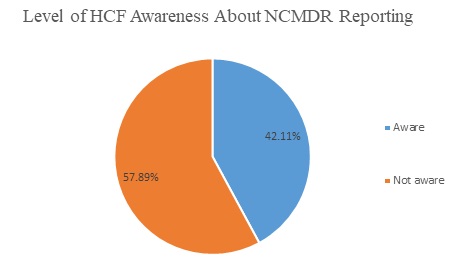
Figure 3: Level of HCF Awareness about NCMDR regarding reporting complaints.
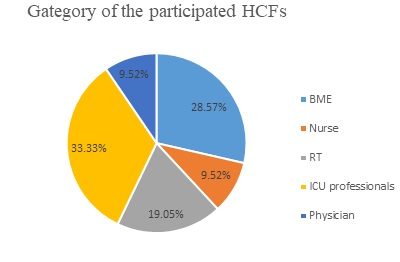
Figure 4: Classifications of the participated healthcare professions.
This study is authored by Eng. Jumana Masoudi, who designed the survey, collected and analyzed data, and wrote up the manuscript of the study. Eng. Abdulmohsen Al-Hajlan verified the study methodology and supervised the study progress. With the appreciation to the post-market clinical evaluation team for their efforts in conducting this work.
For further information or inquiries related to this study, you may contact us at: cia.md@sfda.gov.sa
[1] Kalanuria AA, Mirski M, Ziai W. 2014. Ventilator-associated pneumonia in the icu. Annual Update in Intensive Care and Emergency Medicine 2014.65-77.
[2] Balkhy HH, Cunningham G, Chew FK, Francis C, Al Nakhli DJ, Almuneef MA, Memish ZA. 2006. Hospital-and community-acquired infections: A point prevalence and risk factors survey in a tertiary care center in saudi arabia. International journal of infectious diseases. 10(4):326-333.
[3] Almuneef M, Memish ZA, Balkhy HH, Alalem H, Abutaleb A. 2004. Ventilator-associated pneumonia in a pediatric intensive care unit in saudi arabia: A 30-month prospective surveillance. Infection Control & Hospital Epidemiology. 25(9):753- 758.
[4] Alshamrani MM, El-Saed A, Alsaedi A, El Gammal A, Al Nasser W, Nazeer S, Balkhy HH. 2019. Burden of healthcare-associated infections at six tertiary-care hospitals in saudi arabia: A point prevalence survey. Infection Control & Hospital Epidemiology. 40(3):355-357.
[5] Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C. 1999. The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. American journal of respiratory and critical care medicine. 159(4):1249- 1256.
[6] Fagon J-Y, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. 1993. Nosocomial pneumonia in ventilated patients: A cohort study evaluating attributable mortality and hospital stay. The American journal of medicine. 94(3):281-288.
[7] Al-Dorzi HM, El-Saed A, Rishu AH, Balkhy HH, Memish ZA, Arabi YM. 2012. The results of a 6-year epidemiologic surveillance for ventilator-associated pneumonia at a tertiary care intensive care unit in saudi arabia. American journal of infection control. 40(9):794-799.


